seb derm face wash
 How I cleared up my Serborrheic Dermatitis : SebDerm
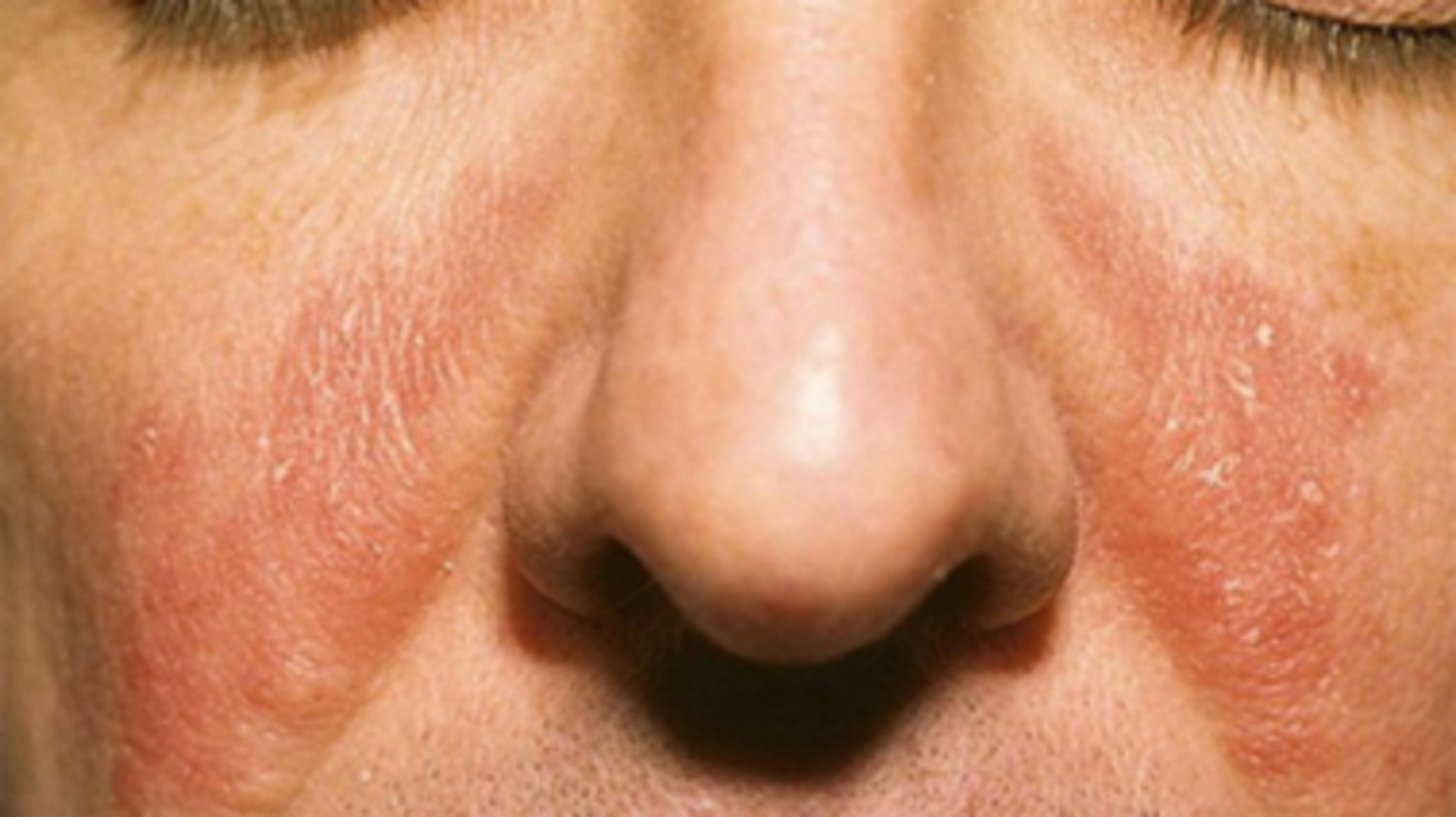
How I cleared up my Serborrheic Dermatitis : SebDermAFP IssuesAFP By Topic Collections AFP CME QuizAFP Community BlogSubscribe to AFPTreatment of Seborrheic Dermatitis. BETTY ANNE JOHNSON, M.D., PH.D., and JULIA R. NUNLEY, M.D., Medical College of Virginia Campus of Virginia Commonwealth University, Richmond, VirginiaAm Fam Physician. 2000 May 1;61(9):2703-2710. Patient information: See the related brochure, written by the authors of this article. Article SectionsSeborreic dermatitis is a chronic inflammatory disorder that affects the areas of the head and trunk where the sebaceous glands are more prominent. The lithophyllous yeasts of the Malassezia gender, as well as genetic, environmental and general health factors, contribute to this disorder. The seborrine of the scalp varies from mild dandruff to dense, diffuse and adherent scale. Facial seborrine and trompa is characterized by a scale of powder or grasient in skin folds and along the margins of the hair. Treatment options include the application of selenium sulfide, pirition cinc, or shampoo containing ketoconazole, topical cetoconazole cream or terbinefine solution, topical sodium sulfate and topical corticosteroids. The etiology of seborreic dermatitis remains unknown, although many factors, even hormonal, have been involved. This chronic inflammatory skin disorder is usually limited to areas of the head and trunk where the sebaceous glands are more prominent. When seborreic dermatitis occurs in the neonatal period, it usually disappears from six to 12 months of age, suggesting that it can be a response to maternal hormonal stimulation. Seborreic dermatitis frequently affects people in post-pubery. Research shows that human sebocy responds to androgen stimulation. Pityrosporum ovale, a lypophilic yeast of the Malassezia genus, has been involved in the development of this condition. It has been suggested that seborreic dermatitis is an inflammatory response to this organism, but this remains to be proved. P. ovale is present in all people. Why do some people develop seborreic dermatitis and others are not unclear? The rate of colonization of the skin involved by this body can be lower than that of the uninvolved skin. However, the fact that seborreic dermatitis responds to antifungal drugs is strongly suggestive of the role of yeast in this disorder. Genetic and environmental factors, as well as other comorbid diseases, may predispose specific populations to the development of seborreic dermatitis. Although seborreic dermatitis affects only 3 per cent of the general population, the incidence in people with acquired immunodeficiency syndrome can be as high as 85 per cent. The exact mechanism by which human immunodeficiency virus infection promotes an atypical and explosive appearance of seborrheic dermatitis (and other common inflammatory skin disorders) is unknown, but many factors have been explored, including T lymphocyte counts with positive CD4, Oval P density and nutritional factors. People with central nervous system disorders ( Parkinson's disease, cranial nerve paralysis, important truncale paralysis) also seem to be prone to the development of seborreic dermatitis, tend to develop a more extensive disease and are frequently refractory to treatment. Seborreic dermatitis in these patients has been predicted to be the result of an increase in sealsity caused by immobility. This growing sebum pool allows the growth of P. ovale, which induces seborrheic dermatitis. Clinical manifestationsSeborreic dermatitis typically affects areas of the skin where the sebaceous glands appear in high frequency and are more active. The distribution is classically symmetrical, and common participation sites are the hairy areas of the head, including the scalp (), the scalp margin (), eyebrows, eyelashes, mustache and beard. Other common sites are the forehead (), nasolabial folds (), external ear canals () and post-auricular folds. The seborrhea of the trunk may appear in the presternal area () and in the folds of the body, including the axill, the navel, the English, and in the inframamary and abnormal areas. It illustrates the typical symmetrical distribution of seborreic dermatitis. FIGURE 1.Seborreic dermatitis of the scalp. FIGURE 1.Seborreic dermatitis of the scalp. FIGURE 2.FIGURE 2.Seborreic dermatitis of the scalp margin. FIGURE 2.FIGURE 2.Seborreic dermatitis of the scalp margin. FIGURE 3.Figure 3.Darrheic dermatitis of the forehead. FIGURE 3.Figure 3.Darrheic dermatitis of the forehead. FIGURE 4.Figure 4.Nasolabial folds. FIGURE 4.Figure 4.Nasolabial folds. FIGURE 5.Seborreic dermatitis of the external auditory duct. FIGURE 5. FIGURE 5.Seborreic dermatitis of the external hearing duct. FIGURE 6.Figure 6.Seborreic dermatitis of the presternal area of the chest. FIGURE 6.Figure 6.Seborreic dermatitis of the presternal area of the chest. FIGURE 7. Symmetric distribution of seboretic dermatitis in the head (top) and body (low). FIGURE 7. Symmetric distribution of seboretic dermatitis in the head (top) and body (low). One of the characteristics of seborreic dermatitis is dandruff, characterized by a thin powdered white scale on the scalp. Many patients complain about the scalp itching with dandruff, and because they think the scale is coming from dry skin, they decrease the rate of shampoo, which allows a larger accumulation. The inflammation then occurs and its symptoms get worse. The most severe seborreic dermatitis is characterized by erythematous plates frequently associated with the powder or greasy scale in the scalp (), behind the ears () and other parts of the distribution described above. In addition to a spicy scalp, patients may complain of a burning sensation in the facial areas affected by seborrhea. The seborrine becomes evident often when men grow moustaches or beards and disappears when facial hair is removed. If not treated, the scale can become thick, yellow and fat and, occasionally, a secondary bacterial infection may occur. FIGURE 8.FIGURE 8.Several seboretic dermatitis of the scalp manifested by dense scale plates. FIGURE 8.FIGURE 8.Several seboretic dermatitis of the scalp manifested by dense scale plates. FIGURE 9.FIGURE 9.Seborreic dermatitis behind the ear, manifested by a scale plate. FIGURE 9.FIGURE 9.Seborreic dermatitis behind the ear, manifested by a scale plate. Seborreic dermatitis is more common in men than in women, probably because the activity of the sebaceous gland is under androgen control. Seborrhea usually appears first in people of its teens and twenty years old and usually follows a course of waxing/requiring throughout adulthood. UV-A and UV-B light inhibits P. ovale growth, and many patients report improvements in seborrine during the summer. Treatment TREATMENT OVERVIEW Hygiene issues play a key role in controlling seborreic dermatitis. Frequent cleaning with soap removes the oils from the affected areas and improves the seborrine. Patients should be advised that good hygiene should be a permanent commitment. Outdoor recreation, especially during the summer, will also improve seborrhea, although caution should be taken to avoid damage to the sun. The pharmacological treatment options for seborreic dermatitis include antifungal preparations (sulfuro of thatlenium, pirition cinc, azole agents, sodium sulfate and topical terbinafine) that reduce colonization by lippophilic yeast and anti-inflammatory agents (topic steroids). Suggested products are listed in . For severe diseases, keratolithic acids such as salicylic acid or coal tar preparations can be used to remove the dense scale; then topical steroids can be applied. Other options for the elimination of the adhesive scale involve the application of any of a variety of oils (peanut, olive or mineral) to smooth the scale during the night, followed by the use of a detergent tar or coal tar shampoo. As a last resort in refractory disease, sebosuppressive agents such as isotretinoin (Accutane) can be used to reduce the activity of the sebaceous gland. Max. For preparations of scalp, apply to night scalp until the inflammation is cleared, then 1 to 3 times per week as required3 by 15 g (Cortaid, 1%) 3 by 15 g (Cortizone 10) 12 by 15 g (Tridesilon) 25 by 30 g (Hytone) 18 by 120 mL (Derma-smoothe/GS Topical oil) Other preparations Sodium sulfacetamide Apply once or twice a daySebizon (10% lot)NoX‡X‡X24 by 85 g (Sebizon)Novacet (10% sulfacetamide sodium plus 5% sulfur)NoX‡X‡X‡X‡X28 for 30 g (Novacet) butSulfacet R Lotion (10% sodium sulfacetamide plus 5% azuX‡X‡ X-ray, x-ray. For preparations of scalp, apply to night scalp until the inflammation is cleared, then 1 to 3 times per week as required3 by 15 g (Cortaid, 1%) 3 by 15 g (Cortizone 10) 12 by 15 g (Tridesilon) 25 by 30 g (Hytone) 18 by 120 mL (Derma-smoothe/GS Topical oil) Other preparations Sodium sulfacetamide Apply once or twice a daySebizon (10% lot)NoX‡X‡X24 by 85 g (Sebizon)Novacet (10% sulfacetamide sodium plus 5% sulfur)NoX‡X‡X‡X‡X28 for 30 g (Novacet) butSulfacet R Lotion (10% sodium sulfacetamide plus 5% azuX‡X‡ Apply to the affected area for 5 to 10 minutes; then rinse; you can bleaching clothes or hairBenzac AC Wash (2.5%, 5%, 10%)NoX21 to 26 by 240 mL (Benzac AC Wash)Benzac W Wash (5%, 10%)NoX21 to 23 by 240 mL (Benzac W Wash)Desquam-X Wash (5% based, 10%)NoX15 to 16 - Top Montvale, N.J.: Medical Economics Data, 1999. The cost for the patient can be greater.† —It can cause atrophy of the skin and telangiectasis with chronic use.‡ - It may not be cosmetically acceptable to some patients. Max. For preparations of scalp, apply to night scalp until the inflammation is cleared, then 1 to 3 times per week as required3 by 15 g (Cortaid, 1%) 3 by 15 g (Cortizone 10) 12 by 15 g (Tridesilon) 25 by 30 g (Hytone) 18 by 120 mL (Derma-smoothe/GS Topical oil) Other preparations Sodium sulfacetamide Apply once or twice a daySebizon (10% lot)NoX‡X‡X24 by 85 g (Sebizon)Novacet (10% sulfacetamide sodium plus 5% sulfur)NoX‡X‡X‡X‡X28 for 30 g (Novacet) butSulfacet R Lotion (10% sodium sulfacetamide plus 5% azuX‡X‡ xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx Other preparations Sodium sulfacetamide Apply once or twice a daySebizon (10% lot)NoX‡X‡X24 by 85 g (Sebizon)Novacet (10% sulfacetamide sodium plus 5% sulfur)NoX‡X‡X‡X‡X28 for 30 g (Novacet) butSulfacet R Lotion (10% sodium sulfacetamide plus 5% azuX‡X‡ Apply to the affected area for 5 to 10 minutes; then rinse; you can bleaching clothes or hairBenzac AC Wash (2.5%, 5%, 10%)NoX21 to 26 by 240 mL (Benzac AC Wash)Benzac W Wash (5%, 10%)NoX21 to 23 by 240 mL (Benzac W Wash)Desquam-X Wash (5% based, 10%)NoX15 to 16 - Top Montvale, N.J.: Medical Economics Data, 1999. The cost for the patient can be greater.† —It can cause atrophy of the skin and telangiectasis with chronic use.‡ - It may not be cosmetically acceptable to some patients. SCALA AND BEARD TREATMENT A lot of cases of seborreic dermatitis are effectively treated by daily shampoo or every other day with antidandruff shampoo containing 2.5 percent sulfur or 1-2 percent of zinc pirition. Alternatively, ketoconazole shampoo can be used. The shampoo should be applied to the scalp and beard areas and leave in place for five to 10 minutes before rinsing. A hydrating shampoo can then be used to prevent hair desication. After the disease is under control, the rate of shampoo with medicated shampoo may be decreased twice weekly or as necessary. The topical terbinephine solution, 1 percent, has also been shown to be effective in treating the seborrhea of the scalp. If the scalp is covered with a diffuse, dense scale, the scale can be removed first by applying hot mineral oil or olive oil to the scalp and washing several hours later with a detergent such as a plate washing liquid or a tar shampoo. An alternative is a night-time application of a tarkeratolytic combination of coal or phenol-saline solution with or without occlusion with a plastic shower cap followed by shampoo in the morning. The extended scale with associated inflammation can be treated by moisturizing the scalp and then applying fluocinolone acetonide, 0.01 percent in oil, to the entire scalp, covering during the night with a shower cap and shampoo in the morning. This treatment can be done at night until the inflammation is cleared and then decreases to one to three times a week as needed. Topic corticosteroid solutions, lotions or ointments can be used once or twice a day for one or three weeks instead of the nightly application of fluocinolone acetonide and can be stopped when itching and erythema disappear. The corticosteroid application can be repeated daily for one or three weeks until the picor and erythema disappear, and then used as necessary. Maintenance with an antidandruff shampoo can be suitable. Patients should be advised to use powerful topical steroids spatically because excessive use can lead to skin atrophy and telangiectasis. Babies often have seborreic dermatitis, commonly referred to as a "cot cap". Areas of possible participation include scalp, face and intertwined areas. Intervention may be extensive, but this disorder is often spontaneously clarified from six to 12 months old and is not repeated until the beginning of puberty. A scalp in a prepuberal child is usually caused by the thynea capitis, not seborreic dermatitis. Therapy for childhood seboretic dermatitis includes frequent shampoo with antidandruff shampoo. If the scale is extensive in the scalp, the scale can be smoothed with oil, gently brushed with a hairbrush and then washed clear. Daily shampoo cannot be reasonable for some populations, such as black people or institutionalized people. In general, weekly shampoo is recommended for black people. As a substitute for daily washing, fluocinolone acetonide, 0.01 percent in oil, can be used as a scalp. Other options include the application of a medium-to-middle-powered topic corticosteroid on a ointment base. As with other forms of therapy, these agents are used every day or twice a day until the condition improves. Subsequently, topical corticosteroids are used as necessary to maintain the condition under control. After initial control is reached, the acetonide fluocinolone, the 0.01 percent shampoo (SAT sheet), can be used as an alternative to fluocinolone acetonide, 0.01 percent in oil (Derma-Smoothe/FS), for maintenance. FEACE TREATMENTThe areas involved in the face can often be washed with shampooes that are effective against seborrhea as detailed above. Alternatively, ketoconazole cream, 2 percent, can be applied once or twice a day to affected areas. Often, 1 percent of the hydrocortisone cream will be added once or twice a day to the affected areas and will assist with the resolution of erythema and itching. Sodium sulfacetamide, 10 percent lotion, is also an effective topical agent for seborreic dermatitis. BODY TREATMENTThe seborrhea of the trunk can be treated with the frequent application of zinc cinc or coal tar containing shampoo or washing with zinc soap. In addition, the topic cream of cetoconazole, 2 percent, and/or a topical cream of corticosteroids, lotion or solution applied once or twice a day will be useful. Benzoyl peroxide washes are also useful for controlling the seborrhea of the trunk. Patients should be warned to rinse thoroughly after the application of these agents, as they will whiten her bed linen and clothes. These agents may be drying, and the patient may benefit from the application of a humectant after treatment. SEBORRHEA TREATMENTAn occasional patient with severe seborrhea that does not respond to the usual topic therapy may be a candidate for isotretinoin therapy. Isotretinoin may induce up to 90% reduction in the size of the sebaceous gland, with a corresponding reduction in the production of sebum. Isotretinoin also has anti-inflammatory properties. Treatment with daily doses of isotretinoin as low as 0.1 to 0.3 mg per kg can result in an improvement in severe seborrhea after four weeks of therapy. Subsequently, a dose as low as 5 to 10 mg a day can be effective as maintenance therapy for several years. However, isotretinoin has potentially serious side effects and few patients with seborrhea are suitable candidates for therapy. The most devastating side effect is teratogenicity, but other serious side effects include hyperlipidemia, neutropenia, anemia, and hepatitis. Mucocutaneous adverse effects include chemotherapy, xerosis, conjunctivitis, uretritis and hair loss. Long-term use has been associated with the development of skeletal hyperostosis idiopathic diffuse (DISH). This agent should be used cautiously and only by doctors who are well versed in all their adverse effects. A more practical approach for the refractory patient can first be to try different combinations of the usual agents: a dandruff shampoo, an antifungal agent and a topical steroid. If this fails, the short-term use of a more potent topical steroid in a "pharmac" can put some refractory patients in the remission and actually decrease the total exposure of steroids. Therapeutic options for pulse therapy may include a class III non-fluorated steroid such as breast-suple furoate (Elocon) or an extra-potent class I or class II topical steroid such as clobetasol (Temovate) or fluocinonide (Lidex). The class III topical steroid should be tested first, but if the condition remains unresponsive, the clinician can then choose to use a class I agent. These more powerful agents can be applied once or twice a day, even in the face, but they must be detained after two weeks due to the increased frequency of side effects. If the patient responds before the two-week limit, the agent must be arrested immediately. Adjuvant therapy including the use of a dandruff shampoo, an antifungal agent, or both, is essential during the "pulse" period and should continue as maintenance therapy after each pulse. Most corticosteroids are available as solutions, lotions, creams and ointments. The patient and the treatment site often determine which vehicle to use. Lotions and creams are often used in all areas of the face and body, while solutions and ointments are most commonly used in the scalp. In general, the application of a scalp solution is preferred by white and Asian patients, but it can be too dry for black patients. Ointments can be a better choice. The vehicle affects the power of a topical steroid. In most circumstances, the same steroid in an ointment is more potent than the steroid in a cream, which in turn is more potent than the same chemical in a lotion. When patients should be referred to a dermatologist if the diagnosis is in doubt or if they do not respond to the treatment. Seborrine may be difficult to distinguish from atopic dermatitis, psoriasis, rosacea or superficial fungal infections. Chronic treatment with topical corticosteroids can lead to permanent changes in the skin, such as atrophy and telangiectasia. The explosive appearance of seborreic dermatitis in a young patient should give rise to the consideration of the infection of the underlying human immunodeficiency virus. Referral to a dermatologist for patients with severe seborrene in which oral isotretinoin treatment is contemplated, particularly if long-term therapy is likely to be needed. Read the full article. Read the full article. Already a member/subscriber? Purchase Access: Already a member or subscriber? Best Value! Get full access from $140 Access This Issue$39.95 Access This Article$20.95 $(."ui-dialog.ui-widget.ui-widget-content.ui-corner-all.subscriptionmodal.ui-draggable").addClass("dept"); Already a member or subscriber? The best value! Get full access This problem Access to this article $(."ui-dialog.ui-widget.ui-widget-content.ui-corner-all.subscriptionmodal.ui-draggable").addClass("dept"); The AuthorsBETTY ANNE JOHNSON, M.D., PH.D., is an associate professor at the General Medicine Division, Virginia Campus Medical College of the Commonwealth University of Virginia, Richmond. He also runs the University of Virginia Commonwealth Student Health Services. She received her medical diploma at Harvard Medical School, Boston, completed her internship of medicine and residence in Brigham and the Women's Hospital in Boston, and received her doctorate in microbiology from the University of Iowa, Iowa City....JULIA R. NUNLEY, M.D., is an assistant professor at the Department of Dermatology, Virginia Campus Medical University Commonwealth University. She received her medical degree at Case Western Reserve University School of Medicine, Cleveland, completed an internship and residency in internal medicine, a invitation in nephrology and a residency in dermatology at the Medical College of Virginia Campus of Virginia Commonwealth University. Correspondence address to Betty Anne Johnson, M.D., Ph.D., Box 980102, Medical College of Virginia Campus of Virginia Commonwealth University, Richmond, VA 23298-0230. The prints are not available from the authors. The authors recognize the assistance of Charles Shasky, R.Ph., M.B.A. and Patricia Bridgers, R.Ph., in the revision of the manuscript. REFERENCES1. Janniger CK, Schwartz RA. Seborreic dermatitis. I'm Doctor Fam. 1995;52:149–55[published erratum appears in Am Fam Physician 1995;52:782]....2. Zouboulis CC, Xia L, Akamatsu H, Seltmann H, Fritsch M, Hornemann S, et al. The model of culture of the human sebocy provides new ideas on the development and management of seborrhoea and acne. Dermatology. 1998;196:21–31.3. There's RJ, Graham-Brown RA. Seborrhoeic dermatitis: causes and management. Dermatol Clin Exp Exp. 1997;22:3-6.4 Parry Yo, Sharpe GR. Seborreic dermatitis is not caused by an immune response altered to malasezia yeast. Br J Dermatol. 1998;139:254–63.5. Schaub NA, Drewe J, Sponagel L, Gilli L, Courvoisier S, Gyr N, et al. Is there a relationship between risk groups or initial T CD4 cell counts and prevalence of seborreic dermatitis in HIV-infected patients? Dermatology. 1999;198:126–9.6. Schechtman RC, Midgley G, There's RJ. Malassezia's HIV and yeast disease: a quantitative study of patients with seborrhoeic dermatitis. Br J Dermatol. 1995;133:694-8.7. Basset-Seguin N, Sotto A, Guillot B, Jourdan J, Guilhou JJ. Zinc status in HIV-infected patients: relation to the presence or absence of seborreic dermatitis. J Am Acad Dermatol. 1998;38:276-8.8. Cowley NC, Farr PM, Shuster S. The permissive effect of sebum on seborreic dermatitis: an explanation of eruption in neurological disorders. Br J Dermatol. 1990;122:71-6.9. Wikler JR, Janssen N, Bruynzeel DP, Nieboer C. The effect of UV light on pityrosporum yeasts: ultrastructural changes and growth inhibition. Acta Derm Venereol. 1990;70:69–71.10. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of seborrhoeic dermatitis and dandruff with ketoconazol shampoo 2%: results of a multicentric, double-blind, placebo-controlled trial. Br J Dermatol. 1995;132:441-5.11. Faergemann J, Jones JC, Hettler O, Loria Yes. Pityrosporum ovale (Malassezia furfur) as a leading agent of seborrhoeic dermatitis: new treatment options. Br J Dermatol. 1996;134 suppl46: 12-538.12. Habif TP. Clinical dermatology: a color guide for diagnosis and therapy, 3d ed. San Luis: Mosby, 1996:214.13. Arndt KA, Bowers KE, Chuttani AR. Manual of dermatologic therapeutics: with essential elements of the diagnosis, 5o ed. Boston: Little, Brown, 1995:166.14. Orphans CE, Zouboulis CC. Oral retinoids in the treatment of seborrhoea and acne. Dermatology. 1998;196:140-7. Copyright © 2000 by the American Academy of Family Physicians. This content is owned by AAFP. A person who sees it online can make an impression of the material and can use that impression only for his personal and non-commercial reference. This material cannot be downloaded, copied, printed, stored, transmitted or reproduced in any medium, either now known or later invented, except as authorized in writing by AAFP. Contact for copyright questions and/or permission requests. You want to use this article somewhere else? More in AFPRelated ContentMore in PubmedMOST RECENT ISSUEMar 1, 2021Mar 1, 2021Acceder to the latest issue of American Family PhysicianEmail Alerts Don't miss a single problem. Subscribe to the AFP free content table. Browse this articleContinue reading Previous: Previous: Next: / / / / Treatment of seborreic dermatitis Copyright © 2020 American Academy of Family Physicians. All rights reserved.

How to treat Seborrheic Dermatitis on your face
![B&A] I cured facial sebhorreic dermatitis using a raw honey mask! : SkincareAddiction B&A] I cured facial sebhorreic dermatitis using a raw honey mask! : SkincareAddiction](https://preview.redd.it/at16yhjcoylz.jpg?auto=webp&s=c1a0166d9b7916f69e7d4b67d3caf123e619e97c)
B&A] I cured facial sebhorreic dermatitis using a raw honey mask! : SkincareAddiction

Seborrheic dermatitis: Treatments and advice to fight it - ISDIN
Things You Should Know About Seborrheic Dermatitis - Pharmaceutical Specialties, Inc.
Facial Seborrheic Dermatitis Control Tips for Dry Flaky Skin on the Face and Around the Nose
![Shelfie] Routine to keep Seb. derm at bay : SkincareAddiction Shelfie] Routine to keep Seb. derm at bay : SkincareAddiction](https://i.redd.it/spyvbbuj9cr21.jpg)
Shelfie] Routine to keep Seb. derm at bay : SkincareAddiction

How I Cured my Seborrheic Dermatitis and Prevent It from Coming Back – Reviews and Snaps by Yanjiil S.

Best Face Washes & Soaps For Seborrheic Dermatitis – Treat Seborrheic Dermatitis

How to treat Seborrheic Dermatitis on your face

How I Cured my Seborrheic Dermatitis and Prevent It from Coming Back – Reviews and Snaps by Yanjiil S.
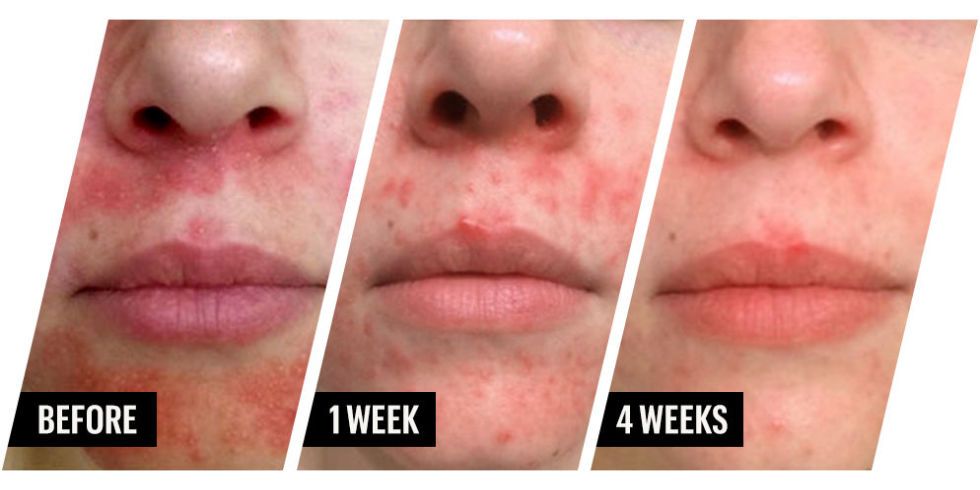
How One Woman Cured Her Acne and Dermatitis with Honey - Honey for Skin Issues

Types of Eczema: Seborrheic Dermatitis | National Eczema Association
![How I cleared up my Seborrheic Dermatitis [B&A] [Skin Concerns] : SkincareAddiction How I cleared up my Seborrheic Dermatitis [B&A] [Skin Concerns] : SkincareAddiction](https://preview.redd.it/fup4yvuf95a11.jpg?width=2048&format=pjpg&auto=webp&s=db4cee7f9071226f693d9a2f059973557996c7d1)
How I cleared up my Seborrheic Dermatitis [B&A] [Skin Concerns] : SkincareAddiction

How I Treat my Seborrheic Dermatitis: Face Edition – The Seborrheic Dermatitis Blog

Seborrhoeic Dermatitis
![Skin Concerns] Seb derm? Rosacea? Both? Other? Not sure where to turn : SkincareAddiction Skin Concerns] Seb derm? Rosacea? Both? Other? Not sure where to turn : SkincareAddiction](https://i.redd.it/wk82oustkwmz.jpg)
Skin Concerns] Seb derm? Rosacea? Both? Other? Not sure where to turn : SkincareAddiction
How to know if worsening dry skin is seborrheic dermatitis | SkinCare Physicians

Woman Used Honey to Cure Her Severe Dermatitis Outbreak | CafeMom.com

Seborrhea | Beautypedia
I lost 24lbs and my skin now shows NO signs of seborrheic dermatitis...none!"* - Juice Master

The Best Moisturizers for Seborrheic Dermatitis (and Sensitive Skin in General!) | Moisturizer for sensitive skin, Seborrheic dermatitis, Sensitive skin

Finally cleared my seb derm! : SebDerm

How to know if worsening dry skin is seborrheic dermatitis | SkinCare Physicians
![8 Best Facial Cleansers for Seborrheic Dermatitis [2021] 8 Best Facial Cleansers for Seborrheic Dermatitis [2021]](https://zelenlife.com/wp-content/uploads/2020/09/CeraVe-Hydrating-Facial-Cleanser-Fragrance-e1600170420206.jpg)
8 Best Facial Cleansers for Seborrheic Dermatitis [2021]

Seborrheic dermatitis Q&A with a dermatologist 🙆🤔 - YouTube

Skincare Routine | Sensitive, Acne Prone with Seborrheic Dermatitis - She's Not A Robot

Seborrhoeic dermatitis | DermNet NZ

Types of Eczema: Seborrheic Dermatitis | National Eczema Association

Dermatologist recommended cleansing bar for acne, blackheads, comedones, rosacea and seb derm. If y… | Rosacea skin care, Dermatologist recommended, Sulfer for acne

Best Moisturizer for Seborrheic Dermatitis on Face - The Derm Report

How to treat Seborrheic Dermatitis on your face

Amazon.com : Seborrheic Dermatitis Cream with Manuka Honey, Coconut Oil and Aloe Vera - Moisturizing Face and Body Anti Itch Cream and Skin for Sensitive Skin - Natural & Organic Cream (4 oz) : Beauty

Seborrheic dermatitis: Natural treatments and remedies

Randy Jacobs, M.D.

I'm 29 years old, diagnosed with seborrheic dermatitis 10 years ago. It destroyed my self esteem and socal life, before it appeared I was popular and extroverted kid. Since than I had

Great Skin Care Tip-Seborrheic Dermatitis - HubPages

Best Face Wash for Seborrheic Dermatitis - The Derm Report

Scalp problems, seborrheic dermatitis & the curly girl method - Charlotta Eve

Bimalar facial rashes - Page 2 of 3 - Clinical Advisor

seborrheic dermatitis blog Vibrant Dermatology & Skinbar MD
Posting Komentar untuk "seb derm face wash"